Of course we don’t want to build Future Fit, a new model for health provision in our area, on fear. But in my view, Future Fit is flawed because it is more theoretical than grounded in the reality of Shropshire’s geography and because I doubt it can be funded.
Yesterday, the Future Fit team held its last major workshop on the future of health provision in Shropshire, Telford and Wrekin and Powys. The event in Ludlow Assembly Rooms was attended by more than 100 people.
As this stage, the discussion is about issues and options. It’s about getting reaction to a set of top down proposals for radical reorganisation of health services including A&E, planned surgery, Minor Injury Units and community hospitals.
The scheme is ambitious and I question whether it is achievable. There will be more care at home and perhaps in GP surgeries – but I did not gain the impression that GPs have been closely involved in this or think they can cope. I heard no mention of carers. The Future Fit model centralises all major operations and significant care needs. It may even lead to a new A&E allied with an Urgent Care Centre midway between Shrewsbury and Telford.
Before I talk more about the options, first let me give a voice to the Future Fit team who have put a lot of effort into these consultations.
Early on in the rather too lengthy proceedings, there was a challenge from the floor:
“Haven’t decisions already been made? That the A&E will go to Telford, the Monkmoor walk-in centre to the Royal Shrewsbury?”
Dr Caron Morton, Accountable Officer of Shropshire Clinical Commissioning Group (CCG) denied this was the case:
“Categorically no decision on A&E has been made. We don’t want to build this model on fear. We can build something very real.”
Later, David Evans, Chief Executive of the Telford and Wrekin CCG also told the audience that decisions have not yet been made:
“I have heard suggestions there may be subterfuge. I completely refute it. It is simply not the case that we have been making decisions behind closed doors. The reason that [Future Fit] feels airy fairy is that it is not yet decided. I know you need answers. What you have heard about today is processes, about the model. If we don’t bring out processes, then [Future Fit] stops being clinical. We are trying to engage with a clinical process and we need your help.”
So what is the Future Fit model? What are these champions of a remodelled health service trying to create? And why is it so controversial?
Future Fit is consulting on six new categories of health facility (see Resource Pack for full details: Future Fit slides):
EC: Emergency Centre. This is A&E to you and me but it will only be accessible via 999 or transfer from an Urgent Care Centre. There will be just one EC, replacing our two current A&Es. It will be at the Royal Shrewsbury (RSH) or Princes Royal (PRH), or a new site somewhere in between. David Evans said: “We know a single EC will deliver better care.”
UCC: Urgent Care Centre. This will be a walk-in facility. Many people will come through referral from 111 or by a medic, or they might arrive by ambulance if the case is urgent but not time critical. There will be a UCC at the RSH and PRH, and a third if a new Emergency Centre site is built. There will be between two and five others. The current Minor Injury Units at Bridgnorth, Ludlow, Oswestry and Whitchurch will close or be upgraded to a UCC. David Evans said: “We need to understand what a UCC delivers and to do that we need to understand what patients need.”
DTC: Diagnostic and Treatment Centre. There will be one of these, possibly located alongside the Emergency Centre. It will deal with planned surgery. This will mean an end to planned operations that are cancelled because of urgent demands from A&E.
LPC: Local Planned Care Services. These services will deal with diagnosis, assessment and follow-up, including tele-consultation with specialists. They will not be stand alone facilities, but attached to UCCs or other health facilities.
CU: Community Units. These will deal with higher acuity than current community hospitals. They will help stabilise and rehabilitate patients. They will probably be located with other facilities and it is not clear how many there will be.
HH: Health Hubs. These seem to be about community empowerment in health, “localised but consistent services.” I am not quite clear what these hubs are or why they are different from what GPs currently provide.
To these six levels of facility we must add GP services, and tertiary specialist hospitals such as Robert Jones at Gobowen. It’s a pretty complex system, isn’t it?
Carol Morton described it as:
“A network model. The beauty of the system at the end is that no health care professional will be operating in isolation, unable to get help from anyone else.”
Future Fit is a big shopping list. It begins with a blank sheet, even to the extent that Carol Morton suggested they would move the newly created Women’s and Children’s Centre from PRH to RSH if the Future Fit model demanded it. That’s nonsense. There would be a monstrous scandal if we scrapped a £28 million purpose built unit for an unproven theoretical model of health provision. But Dr Morton said:
“There are no fixed points. If we put in fixed points, there will be no movement at all.”
That’s one of my major concerns about Future Fit. It seems to assume that we can impose a theoretical model regardless of current provision and infrastructure. We can’t. We have superb facilities we must keep and valued locations where we must maintain a service.
The proposal for a new Emergency Centre (A&E) and UCC site is not viable. It is purely a fudge to prevent the location becoming a political battleground in the run up to the 2015 general election. There is never going to be enough money to build a new facility and it will be unwise to blow any available money on a new site. The new EC it will be located at RSH in Shrewsbury or PRH in Telford. Many people at the meeting thought it will inevitably be in Telford, a hugely difficult place to access by public transport if you live in this part of the county.
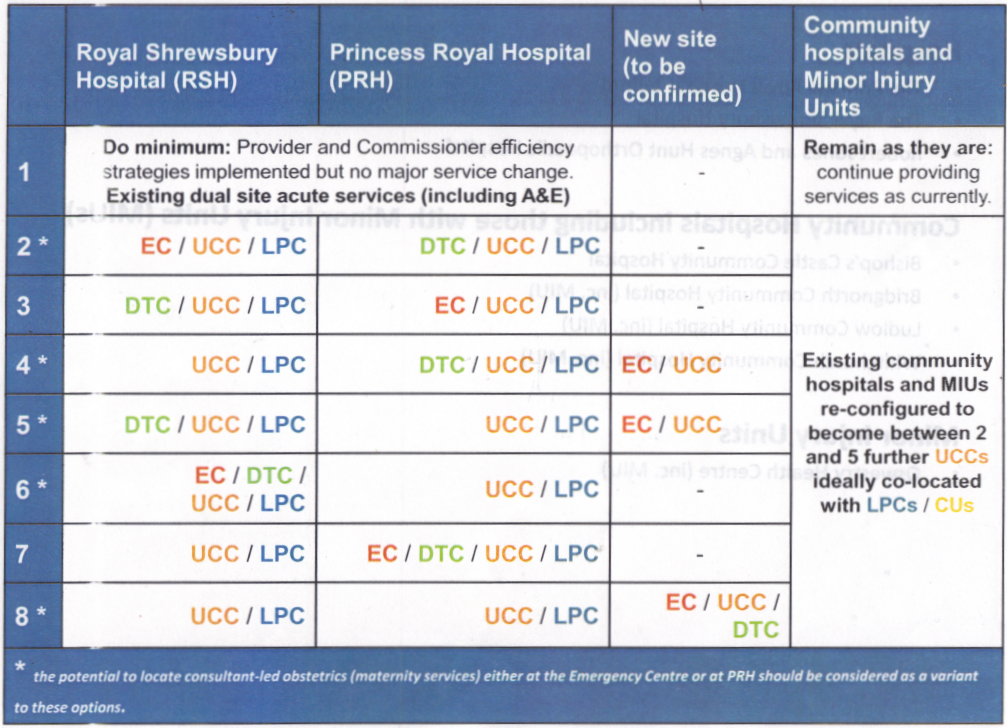 Colocation options for Future Fit
Colocation options for Future Fit
We were told that you get better care in bigger facilities (we don’t seem to call them hospitals any more).
“If care is dispersed,” GP and Future Fit clinical designer Bill Gowans told us, “It is more costly and less good.” I accept that, but if your condition deteriorates or you die on the way to hospital, that better care will be negated. Bill told BBC Radio Shropshire this morning that it is “people that matter not buildings.” That’s right but getting the right locations for treatment is also vitally important.
Access is the critical issue in this rural county. If you live in Bishop’s Castle, have to wait for a blue light ambulance to come from Craven Arms and then get taken to PRH at Telford, that’s a 46-mile trip on lousy roads. Then your friends and relatives need to travel on a nearly 100-mile round trip to see you. To go from my house in Ludlow to PRH, I need to catch two buses and two trains. Distance to medical assistance is a crucial factor in health outcomes and excessive distances discourage people from engaging with health services.
So will we get our community hospital in Ludlow upgraded to an Urgent Care Centre? Carol Morton told us: “The south of the county will have a UCC. Will it have 2 or 3? I can’t say.” That sounds to me like there will only be one UCC in the south, denying either Bishop’s Castle, Ludlow or Bridgnorth local urgent care facilities. If people have to travel long distances to a UCC, they’ll go to our already overloaded GPs instead.
I am concerned that we heard little about GPs, nurses, community nurses and carers at this event. It is clear that they have not been forgotten, but if they are not central to the model they are in danger of being squeezed out the inevitable struggle for resources.
I’m concerned about the bureaucracy too. We are a model with a least eight levels of health facility. This will be confusing and each part of the operation will need its own managers and administrators. The NHS already suffers from excess bureaucracy.
Until questioned by the audience, we heard little about mental health. Bill Gowans told us “No health without mental health” is not just a slogan. The Future Fit team want mental health integrated alongside mental health. Yet, we had to prompt for answers on mental health and it doesn’t seem central to the model.
Future Fit is hugely ambitious. It is prone to failure if three conditions cannot be met. Those conditions are making the best use of existing infrastructure; ensuring local provision across the county; and securing adequate financing.
Yesterday’s workshop was well worth attending and I thank the Future Fit team for organising it. But I think it unfortunate that there were no young people present. It’s their future we are discussing. I am also not convinced that we discussed a system that is financially and operationally viable, or gives enough consideration to the south and rural parts of the county.
