Helen Morgan, MP for North Shropshire, secured an adjournment debate in the House of Commons last Thursday as MPs departed to their constituencies and beyond for the Easter recess. Excluding the deputy speaker, there were just five MPs present. Philip Dunne, Daniel Kawczynski and Mark Pritchard were conspicuous by their absence. Lucy Allen, Tory MP for Telford, did attend.
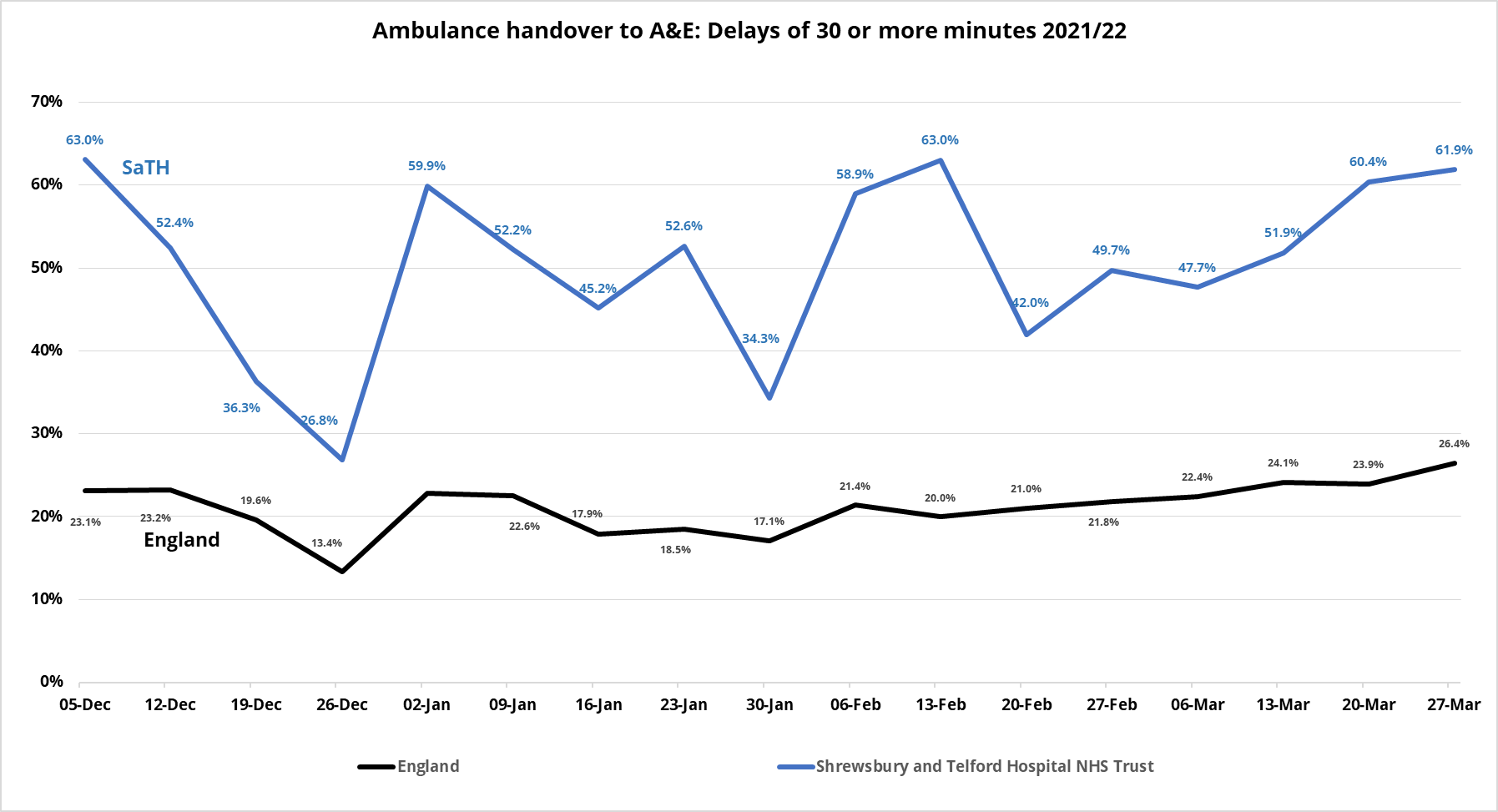
On the day of the debate, NHS England published data showing that ambulance handover times at the Royal Shrewsbury Hospital and Princes Royal Hospital were among the highest in the country. In the last four months:
- 51% of ambulances have been delayed for 30 minutes or more at the two SaTH hospitals compared to 21% across England
- 28% of ambulances have been delayed for 60 minutes or more at SaTH compared to 9% across England.
In recent weeks, handover delays of 30 minutes or more have risen to 62%.
Extracts from the debate [video]:
I am not here to criticise the hard-working NHS staff in our ambulance services and emergency departments. Indeed, I thank them for their incredibly hard and dedicated work in difficult and demotivating circumstances, but there is clearly a problem with the provision of emergency care in Shropshire…
Just since Monday, my office has been met with a tidal wave of correspondence, each story as saddening and frightening as the last. A care home reported a wait of 19 hours for an elderly resident with a broken hip. An elderly diabetic man fell and dislocated his shoulder. He was advised not to drink or eat anything in case surgery was required, and then waited 15 hours for an ambulance to arrive. A disabled man fell in his bathroom and waited for 21 hours for an ambulance. He was fortunately lifted from the floor after eight hours by a helpful neighbour. A man waited with a stranger experiencing heart attack symptoms on the side of the road for hours, only to give up and drive the gentleman to A&E himself.
A man with a suspected stroke waited nine hours for an ambulance and a further five in the ambulance waiting to be transferred into hospital. A 92-year-old lady fell at 8.30 in the morning, suffering bleeding from the head and a broken leg. She was looked after by her 75-year-old neighbour for almost eight hours until the ambulance arrived, and then waited in the ambulance for transfer into the A&E department until 2.30 the next morning. She had not eaten since 6.30 the evening before her fall. An elderly woman fell down the stairs shortly after lunch. After an 11-hour wait, she was alone with her front door open so that the ambulance crew could access her house. That was 3 o’clock in the morning.
I could easily spend the next half hour relating heartbreaking stories…
What all these stories have in common is that they could have been much worse… I know this problem is not unique to Shropshire… In parts of Britain, an excessive wait for an ambulance has become normal…
There are consistent themes at the core of the issue… The first is the problem of handing over patients at the emergency departments in Shrewsbury and Telford. West Midlands Ambulance Service has told me that, on the day [a] young footballer dislocated his knee, 868 hours were lost waiting to hand over patients, and that nearly 2,600 hours were lost in the month up to 29 March. Handover times in Shropshire are significantly worse than in the rest of the country, and there have been times when every ambulance based in Shropshire is waiting outside a hospital to discharge a patient.
The hospital trust has declared a critical incident on no less than four separate occasions so far this year, and each of those incidents coincided with an increase in the number of heartbreaking stories coming into my inbox.
The emergency departments of the Shrewsbury and Telford Hospital NHS Trust report that they suffer from a shortage of space and staff, along with the additional challenges of separating covid patients—on Tuesday this week, the trust had more covid patients than at any previous point in the pandemic. The trust also reports delays in discharging patients who are well enough to leave hospital because it is struggling to find care packages or care home spaces.
The impact of all this is that, because ambulances wait so long at hospitals, the vast majority of ambulance journeys across Shropshire begin in Shrewsbury or Telford. It is not possible to reach the most seriously ill patients towards the edge of the county within the target time if the ambulance sets out from one of those two towns. This, combined with the closure of community ambulance stations, means that very few ambulances are free in places such as Oswestry and Market Drayton when people become ill and require one.
The Government must deliver on their promise to recruit more GPs, and they must ensure that people with non-urgent healthcare needs are provided with adequate resources in the community…
The Government have refused to listen to the countless warnings by campaigners and those working on the frontline. The Care Quality Commission… last year, gave a stark warning that overstretched ambulance services and emergency departments are putting patients at risk…
The hopes of the Shrewsbury and Telford Hospital NHS Trust are pinned on the Future Fit hospital transformation programme, which kicked off in 2013. It is reliant on £312 million of funding, the source of which may be an interest-bearing loan… Unfortunately, more than eight years later, a strategic outline case has still not been signed off. The estimated costs have spiralled by almost 70%…
The initial promises of urgent care centres in more rural areas—for example, one was guaranteed for Oswestry—investment in community hospitals and local planned care centres were all quietly dropped in the summer of 2015. Promises of investment in public health and prevention, which is a good idea and would have been welcome in Shropshire, are also apparently no further forward. We are consistently told that there is no more money in the pot for faster, better-resourced ambulance services or urgent care staff…
The Secretary of State could commission the Care Quality Commission under powers laid out in section 48 of the Health and Social Care Act 2008 to conduct an investigation into the causes and impacts of ambulance service delays… As I have outlined, the causes will most likely lie in a number of areas across emergency and social care, but until they are fully understood by the right people, they cannot be resolved…
I brought this debate to Parliament to ensure that the Minister and the Secretary of State understand the scale of the problem in Shropshire and, crucially, the urgency in resolving it. How many more elderly citizens will have to wait for 10 hours, with their front door open, for an ambulance? How many more people will have to wait at the roadside with a stranger who they believe might be close to death? How many more young adults will develop hypothermia when they initially have a trivial injury, such as a dislocated knee? How many more cases of serious harm, or even avoidable death, will it take?…